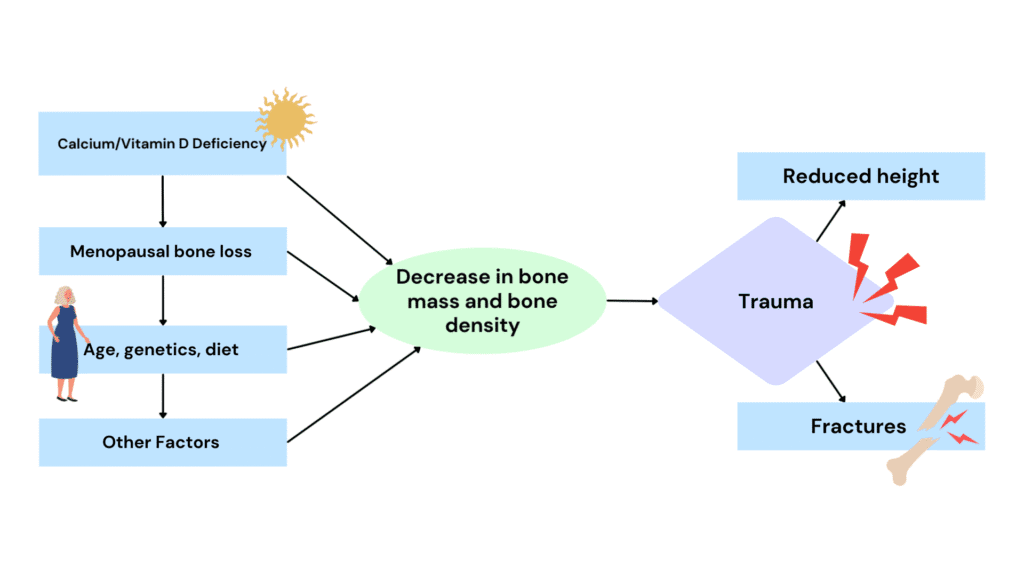
Osteoporosis literally means “bones with holes.” It develops when minerals such as calcium are lost from the bones faster than they can be replaced, leaving them weaker and more fragile.
Hormones play a big role in keeping bones strong. Oestrogen, for example, slows down the activity of cells called osteoclasts, which break down bone. After menopause, oestrogen levels fall, which means osteoclasts become more active and bone is broken down faster than it’s rebuilt. Over time, this loss of bone density can lead to osteoporosis.
Osteopenia is the stage before osteoporosis. It means bone density is lower than normal, but not yet at the point of being classified as osteoporosis.
Both conditions are often called “silent diseases” because you may not know you have them until a fracture occurs. Pain isn’t a symptom of osteoporosis itself – it usually only develops after a break. The first signs are often:
- A reduction in height
- Hip fractures (especially at the neck of the femur)
- Wrist fractures after a fall on an outstretched hand (Colles fracture)
- Vertebral fractures in the spine
It’s important to note that osteoporosis is a disorder of bone mass, not just calcium metabolism.
Other risk factors include:
- Cigarette smoking
- Drinking more than 2 standard alcoholic drinks per day
- Having more than 3 cups of caffeine per day
- Lack of physical activity
- Early onset menopause (before age 45)
- Long-term use of certain medications or conditions such as:
- Thyroid disease or an overactive thyroid gland
- Rheumatoid arthritis
- Chronic kidney and/or liver disease
- Conditions that affect nutrient absorption, including:
- Crohn’s disease
- Coeliac disease
- Inflammatory Bowel Disease (IBD)
- Other gastrointestinal tract conditions
How Can It Be Managed?
Management of osteoporosis is largely centred around prevention and long-term bone health maintenance. The goal is to slow the rate of bone loss, improve bone strength, and minimise the risk of fractures.
The most effective approach is to establish strong bones and muscles from early adolescence through adulthood, as peak bone mass is reached by the late 20s. However, proactive strategies remain beneficial at any age.
Key management strategies include:
- Physical activity: Regular weight-bearing and resistance exercises are essential to stimulate bone growth, improve muscle strength, and support balance – helping to reduce the likelihood of falls and fractures.
- Medical monitoring: Routine check-ups and bone density scans (DEXA scans) allow for early detection and tracking of bone health.
- Lifestyle modification: Reducing smoking, limiting alcohol intake, moderating caffeine, and maintaining a nutrient-rich diet support both bone density and overall health.
- Addressing underlying conditions: Managing chronic illnesses (such as thyroid disorders, coeliac disease, or rheumatoid arthritis) and reviewing the long-term use of medications that may impact bone health are key steps.
Even following diagnosis, osteoporosis can be managed effectively. A structured, individualised rehabilitation program can focus on safe strength-building, postural correction, and fall-prevention strategies. This not only helps preserve independence but also reduces the risk of fractures and related complications in the future.
Dr Katelyn Waring
Osteopath
E: Katelyn.Waring@staytuned.com.au